On an ACEs Connection webinar on Monday, Dr. Andrew Seaman, an assistant professor at Oregon Health & Science University, showed how he navigates his students through the science of adverse childhood experiences (ACEs). And, in an unusual twist for a webinar, Seaman and O’Nesha Cochran, a peer mentor with the Mental Health Association of Oregon, role-played doctor-patient interactions to show how to develop the skills to communicate with patients with high ACE scores.
About 90 people watched “Teaching trauma-informed practices to students and residents in health care fields.” Seaman began with an overview of ACEs science, including showing the links between multiple ACES, injection drug use, alcohol use and suicide attempts, and how the brain becomes less able to manage stress.
For students to truly understand how trauma impacts people’s lives, said Seaman, they need to be able to interact with someone who’s had first-hand experience, and can describe what it’s like to live with trauma.
That’s when Seaman introduced Cochran, who works with patients at Oregon Health & Science University hospital, and trains and coaches students in how to interact with patients who have experienced severe trauma.
Seaman and Cochran role-played doctor-patient interactions to illustrate the nuances of body language, tone of voice and listening skills that can turn a tense, escalating encounter between doctor and patient into one where there’s respect and the possibility of building trust.
This webinar came about after I met Cochran at a conference entitled “Putting Care at the Center” put on by the National Center for Complex Health and Social Needs. She was among the speakers who were invited to talk about how their own histories had shaped the advocacy work they were now doing on behalf of people who had had similar experiences.
Cochran, a peer mentor for patients with substance use addictions, is a pioneer. She was the first person to work in that role at Oregon Health & Science University hospital. She brought to this work her knowledge honed from 22 years of addiction, 15 years in prison, and a childhood, where she explained for an article I did about her and Seaman: “My mom sold me to her tricks and her pimps from the age of three to the age of six.”
At the conference, Cochran had told a story about how one social worker in Oregon who didn’t really understand Cochran’s role, finally heard it first-hand. As the social worker stood in the hallway, Cochran recounts, there was a patient who Cochran said “was screaming and cussing everyone out.” She was the type of patient, Cochran said pointedly, who was typically described as “aggressive and intimidating.”
When Cochran approached the room with the social worker in earshot, another hospital staff person not knowing about Cochran’s work, warned her not to go into the patient’s room. “But I went in and she [the patient] was screaming, I was yelling. She was screaming, I was yelling and it’s getting louder, and then you hear this laughter, right?” she said. At the next staff meeting, Cochran says, the social worker recounted the screaming and then the laughter. “She said, ‘Now I know what you all are doing’.”
When I posted the article about Cochran and Seaman, I had provided Seaman’s email for people who were interested in learning more about their curriculum. After a couple of days of Seaman being deluged with email requests for the curriculum, we decided to do a webinar to show how their approach works, and to make the curriculum available.
Here are bios for O’Nesha Cochran and Dr. Andrew Seaman. You will also find attached Seaman’s and Cochran’s curriculum adapted from what he uses when team-teaching with Cochran; printable trauma-informed practices flash cards; and slides for my introduction to ACEs Connection.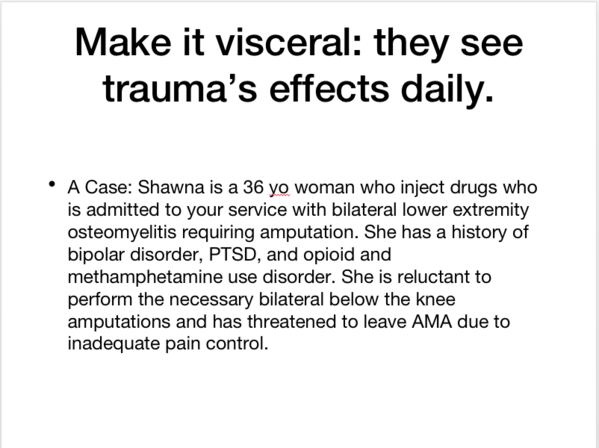
The webinar video begins with Seaman and Cochran role playing a doctor-patient interaction. Prior to using role-play, or as Seaman calls it “skills building,” he advises that the best way to set up role-plays for people who want to learn how to do them is to ask them to observe in what ways the doctor is modeling trauma-informed practices and what they notice about the interaction.
We’d like to encourage the participants and anyone listening to the recording of the webinar to share your comments and questions below. (Here again is a link to the role-playing section of the webinar.)
We'd also like to know if others are doing similar work, so that we can gather as much information about this as possible and make it available to the ACEs Connection community.



Comments (8)