 Take a framework for trauma-informed primary care.... add an in-depth academic overview of ACEs-related research for physicians. Then couple a 50-slide PowerPoint that physicians can use to educate legislators and members of the medical community who still need to be convinced....with a physician journalist's look at how the medical community is creating a dedicated primary care framework that provides room for trauma-informed approaches in health care. And what do you have?
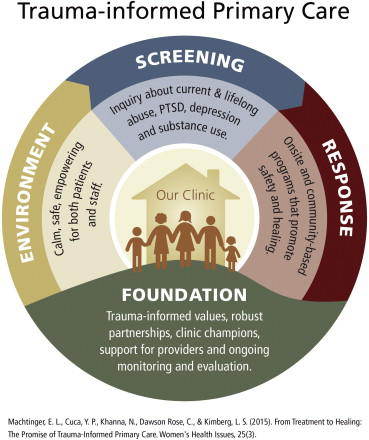
Take a framework for trauma-informed primary care.... add an in-depth academic overview of ACEs-related research for physicians. Then couple a 50-slide PowerPoint that physicians can use to educate legislators and members of the medical community who still need to be convinced....with a physician journalist's look at how the medical community is creating a dedicated primary care framework that provides room for trauma-informed approaches in health care. And what do you have?From Treatment to Healing: The Promise of Trauma-Informed Primary Care — Five clinicians and health care providers from University of California, San Francisco and the Positive Women’s Network in Oakland, CA, developed an approach to trauma-informed primary care that defines trauma broadly, addresses both recent and lifelong trauma, and includes an essential focus on provider support and well-being.
The paper begins:
Janice is a 45-year-old woman with poorly controlled diabetes, obesity, and alcoholism. She feels ashamed about her alcohol use and about her body. She fears that her clinician will be angry with her for not checking her blood sugar, not losing weight, and for missing multiple gynecology appointments. Janice's clinician has worked with her for over a year and is frustrated by their inability to make progress together on her health issues. Janice has never revealed to any of her clinicians that she was sexually abused during childhood nor that she is currently experiencing severe emotional abuse by her husband.
For many people like Janice and her provider, understanding the connection between traumatic experiences and health can be transformative and healing. When patients understand that childhood and adult trauma underlie many illnesses and unhealthy behaviors, they often stop blaming themselves, feel more self-acceptance, and make progress toward health and well-being. Providers who understand this connection are able to create clinical environments that are less triggering for both patients and staff, identify referrals to appropriate trauma-specific services, and develop more effective therapeutic alliances and treatment plans with their patients.
Our strategy group worked to clarify a practical framework for TIPC, a patient-centered approach that acknowledges and addresses the broad impact of both recent and lifetime trauma on health behaviors and outcomes. The goal of TIPC is to improve the efficacy and experience of primary care for both patients and providers by integrating an evidence-based response to this key social determinant of health.
And the paper ends with how Janice's treatment was completely different than what she might receive in a traditional medical practice. It's definitely worth a read.
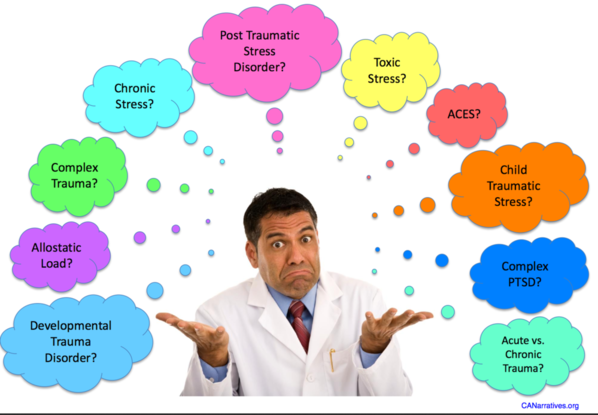
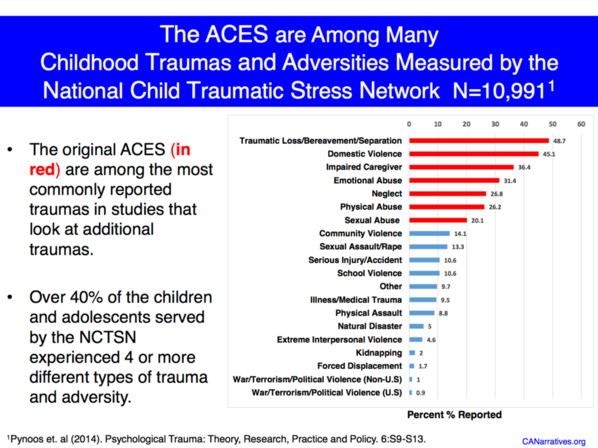
Childhood Adversity Narratives (CAN)— Physicians and ACEs experts from UNC, Duke, UCSF and the New School developed a fabulous 50-slide PowerPoint and PDF that the healthcare community can use to educate policymakers and the public about ACEs. They begin with an explanation of their approach:
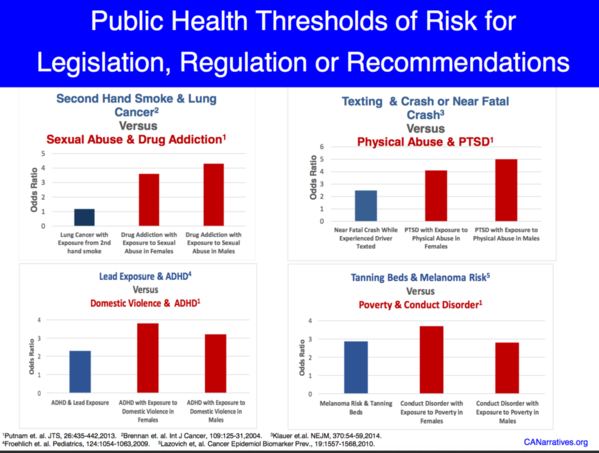
And there's a section of the PPT that looks at synergies, public health thresholds of risk and odds ratios. All fascinating. Here' just one of the slides:
AVA’s ACEs: Informing Best Practices — More than 30 physicians, nurses and other health care providers from the Academy on Violence and Abuse worked two years on this online living document designed to inform healthcare providers who want to address ACEs and other past traumatic stressors in their patients.
Fifteen chapters cover topics such as resilience, clinical approaches for adults, geriatric patients, systems integration, lifetime costs, etc. The chapters are short and concise, and written in academic medical language, with hyperlinked resources so that you don't have to go surfing to find the references. Here's a sample from the chapter on resilience, written by Machelle D. Madsen Thompson, PhD; and Bart Klika, PhD, MSW:
Assessment of ACEs, however, only represents one side of the prevention coin.10 As healthcare providers work to identify and lessen the number and impacts of ACEs, they also should understand the potential sources of protection that can foster resilience for all of their patients. Identifying the presence or absence of protective factors through universal screening allows healthcare providers to make targeted referrals to facilitate the continued development of such factors. For example, if a child’s parent is diagnosed with a medical illness that limits her ability to support the child, the practitioner could identify and encourage other positive adult mentors in the child’s extended family, school, community, or faith group to provide both practical and emotional support. In this way, healthcare providers contribute to the “promotion of safe, stable, and nurturing relationships” and well-being for all children and families.11
A review of more than 200 research articles, coupled with narratives of over 350 adults and children,5 demonstrates that several important protective factors are known to help a child who has experienced multiple ACEs.12,13,14 To aid the healthcare practitioner, each protective factor listed below contains references to information, handouts, and real-world implementation for children and families affected by or at risk for ACEs.6,13
Another bonus is that each chapter comes with a place for people to add their comments. The AVA wants this to be a living document, one that they can regularly update with the latest information.
Overkill — In this update of his 2009 New Yorker article (The Cost Conundrum) on unnecessary medical care, Dr. Atul Gawande explains how some physicians have abandoned a system (including 15-minute appointments) in which they have no chance of getting to the root of patients’ illnesses in favor of the 45-minute appointments of “dedicated primary care”. The physicians are saving Medicare tens of millions of dollars…and they’re making more money.
Here's a short excerpt to whet your appetite:
Then, later that year, officials at a large medical group called WellMed contacted [Dr. Armando] Osio. They wanted to establish a practice in McAllen, catering to Medicare patients, and asked whether he’d join them. WellMed had contracted with Medicare H.M.O. plans to control their costs. Its pitch to clinicians was that, if a doctor improved the quality of care, this would save on costs, and WellMed would share those savings with the doctor in the form of bonuses. That meant Osio would have to see fewer patients, for longer visits, but WellMed assured him that, if he could show measurable quality improvements, he’d actually make more money.
Osio was skeptical, but he agreed to see some of WellMed’s patients. When he was in training, he’d been interested in geriatrics and preventive medicine. In practice, he hadn’t had time to use those skills. Now he could. With WellMed’s help, Osio brought on a physician assistant and other staff to help with less complex patients. He focussed on the sicker, often poorer patients, and he found that his work became more satisfying. With the bonuses for higher patient satisfaction, reducing hospital admissions, and lowering cardiology costs, his income went up. This was the way he wanted to practice—being rewarded for doing right rather than for the disheartening business of churning through more and more people. Within a year, he’d switched his practice so that he was seeing almost entirely WellMed patients.
He gave me an example of one. That day, he’d seen an elderly man who had taken a bad spill two or three weeks earlier, resulting in a contused kidney and a compression fracture of his lower spine. After a couple of days in the hospital, he’d been sent home. But the pain remained unmanageable. He called Osio’s office seeking help.
If the man had called five years ago, a receptionist would have told him that the schedule was full for days and sent him to an emergency room. There, he would have waited hours, been seen by someone who didn’t know his story, been given a repeat CT or MRI, and then likely have been kept for another hospital stay. Once the doctors were sure that the situation wasn’t dangerous, he would finally have been sent home, with pain medicine and instructions to see his primary-care doctor. Cost: a few thousand dollars.
Now when the man called, the receptionist slotted him to see Osio that afternoon. The doctor examined him and, being familiar with his case, determined that he had no worsening signs requiring imaging. He counselled patience and offered reassurance, gave him pain medication, and sent him home, with a plan for his nurse to check on him the next day. Cost: at most, a hundred dollars. And the patient got swifter, better care.
There's so much more. Chock full of good info, and a great read.





Comments (2)