Once again, I was struck by the number of those with the chronic relapsing brain disease of addiction in the audience at a lecture I gave last night who have four or five of the five key risk factors for developing addiction. Not only that, but they had three or four of the five key risk factors BEFORE they had their first drink or drug use experience. And for the majority of them, their risk factors were rooted in the childhood trauma they experienced - the verbal, physical, emotional abuse, neglect - that is often the unintended outcome a child experiences when growing up in a home with untreated, unhealthily discussed substance abuse or addiction or in a home with a parent(s) who didn't abuse drugs or alcohol, themselves, but were raised by a parent who did. Notice I wrote, "unintended."
As someone with over 40 years personal experience with a number of family members and close friends' alcohol abuse and/or alcoholism, I changed. I changed radically. I changed in order to cope with the secondhand drinking (the impacts of their drinking behaviors), and in that change, I became part of the problem because it is a dance, and as with any dance, it takes two doing the same step to the same beat of the same music that makes the dance work. I have learned through my 11 years of research, writing and consulting in this field that people with the disease of addiction are not weak-willed, do not want to harm those they love the most, and have (for the most part) no understanding of the brain disease of addiction they have, nor how to treat it, which is true for the family member, as well, and is how they unwittingly become part of the problem, which contributes to the insanity of "The Dance" and leaves the children in a swirl of childhood trauma.
Now back to my lecture of last night... for all of those present, learning how addiction develops and the role of these five key risk factors in that development was an "ah ha" moment. This is not to tout my lecture. Rather it is to raise awareness that one of the most important ways we can PREVENT substance abuse and/or addiction is to understand the risk factors for developing it in the first place so that we might help the children whose lives we influence.
Which takes me to the point of this post, namely to share one I wrote, titled: "Want to Prevent Addiction? Assess Your Risk Factors," on my blog, February 6, 2014. I have copied and pasted the portion of the post related specifically to the five key risk factors, however the entire post may be of interest, as well.
There are five key risk factors that contribute to a person developing the disease of addiction – genetics, childhood trauma, mental illness, social environment and early use. Please remember – just because you have one or more risk factors doesn’t mean you are one drink or one drug use away from alcoholism or drug addiction. It means you want to be very, very careful in your use of drugs or alcohol because your brain may not interact the way another person’s brain does and the only brain you need to worry about is your own.
Genetics - It’s not that there is a specific addiction gene – at least not one that has not been identified, yet. Rather it’s the idea of genetic differences. There are roughly 25,000 genes in our DNA, and the way they turn on or off determines how we look and how our bodies work. So just as we are born with (inherit from our parents) certain genetic differences that determine our eye shape or skin color, for example, so too are there genetic differences, such as higher or lower levels of dopamine receptors or lower levels of the enzymes in the liver that break down the alcohol in one standard drink, that can influence how one person’s brain or body will interact with the chemicals in alcohol or drugs. These genetic differences are passed along from one generation to the next. So looking at your family history – mom, dad, grandparents, siblings, aunts/uncles – to see if they had/have addiction is one way to determine if you are predisposed to it, as well. According to the National Institute on Alcohol Abuse and Alcoholism (NIAAA) > Genetics of Alcohol Use Disorders, “genes are responsible for about half of the risk for alcoholism.”
Mental Illness – Mental illnesses, such as depression, anxiety, bipolar, PTSD, ADHD, are also brain changers / brain differences. In other words, the way a person with mental illness’s brain cells communicate with one another is different (for a variety of reasons) than someone who does not have one. This is important to understand because ”[t]hirty-seven percent of alcohol abusers and 53 percent of drug abusers also have at least one serious mental illness,” reports the National Alliance on Mental Illness (NAMI). To learn more about mental illnesses, check out the NAMI > Mental Illness (there you will find detailed information on various kinds of mental illnesses, as well treatment options).
Childhood Trauma – Childhood trauma has a profound impact on the neural circuitry of a child’s brain (meaning how or if brain cells “talk” to one another). It “injures a child’s brain. It impairs the brain’s physical development and function. You can see the effects of trauma on a brain scan,” writes ACEs Too High, a fantastic organization working to raise awareness and mitigate the consequences of ACEs (Adverse Childhood Experiences – childhood trauma). This in turn has a profound impact on how a child copes – how they express anger, fear, powerlessness, how they interpret and respond to other people’s words and actions, how or if they trust, how they learn – it can even lead to mental illnesses, such as anxiety and depression. These brain changes in turn have a profound impact on whether that child’s brain will seek drugs or alcohol for their brain-soothing qualities, as well as how that child’s brain will interact with drugs and alcohol if they use.
Childhood trauma includes verbal, physical and emotional abuse and sexual abuse, for example. It also includes domestic violence in the home and parental divorce. For more on ACEs, visit ACEs Too High and visit the source of this research, the ACE Study, which was a collaboration of the Centers for Disease Control (CDC) and Kaiser Permanente’s Health Appraisal Clinic in San Diego involving over 17,000 Kaiser patients.
Social Environment – If a person lives or works or goes to school in an environment where heavy drinking or drug use is the norm, that person will likely drink or use drugs to that same level. Unfortunately, that same level may not work in their brains the way it works in the brain of their co-workers, family members, fellow students or friends (and frankly, it’s likely not working all that well in those other brains, either). To learn more about what is considered “normal” or “low-risk” drinking, visit NIAAA’s website, Rethinking Drinking. As for “normal” or “low-risk” drug use, visit Single Question Drug Screen – Abuse | Addiction.
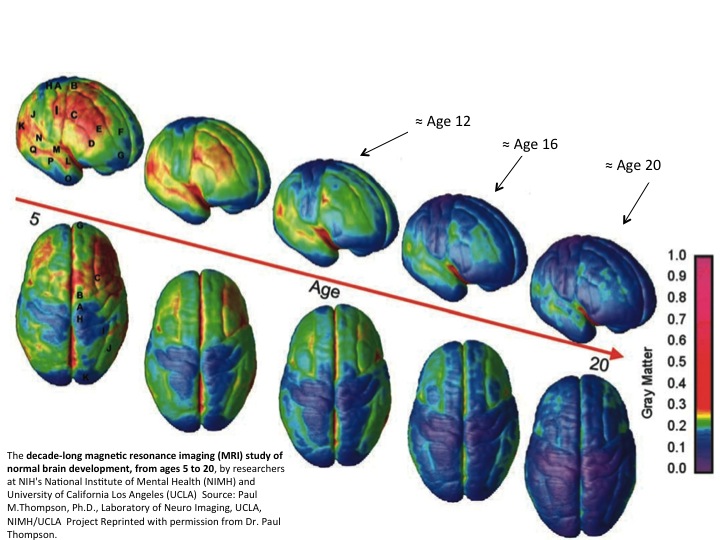
Early Use - This is incredibly important to understand because the adolescent brain is not the brain of an adult. That means the adolescent brain reacts differently with drugs and alcohol than the brain of an adult AND the harm of substance abuse during key developmental processes makes adolescent substance abuse ESPECIALLY problematic.
Dr. Paul Thompson’s 10-year time lapse study of brain development ages 5-20 shows just how much wiring – brain maturity – occurs from approximately ages 16-20. It’s now understood this maturity process continues until roughly age 25.Telling the adolescent brain, ages 12-15, to “just say ‘no’” doesn’t work because the adolescent brain is telling the adolescent to “take risks,” “turn to your peers,” and if their peers are saying, “yes” to risks, drugs and/or alcohol, likely that adolescent will, too. This does not mean they’re a bad kid; it simply means their brain’s instinctual wiring (that which activates during puberty) is in charge. The Partnership at Drug Free.org’s Guide to the Teen Brain>Why Teens Act This Way explains this science.
Lastly, early use – early abuse of drugs or alcohol – wires in brain maps around the finding, seeking, using, hiding, covering up, recovering from at an especially vulnerable time because it’s occurring during the time the brain is going through it’s CRITCAL cerebral cortex development and its strengthening and pruning processes. For more on this, please check out Underage Drinking – How Teens Can Become Alcoholics Before Age 21 and It’s Time to Tell the Whole Truth About Puberty
Click here to read the rest...



Comments (0)