School and city leaders in Hancock County, TN, agree to become a pilot for the Ballad Health Strong Starts for Schools program.
______________________________________
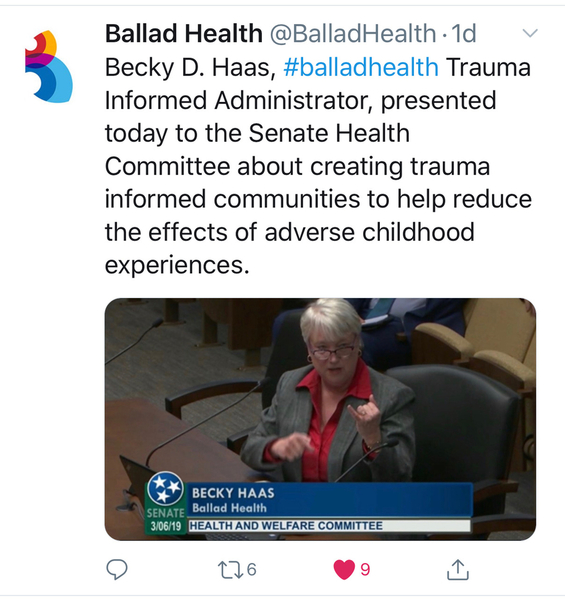
Slowly, but at warp speed. That’s what it feels like to take on educating 16,000 staff member in 21 hospitals that serve 29 counties, says Becky Haas, trauma-informed administrator for Ballad Health. Ballad Health is a healthcare organization that serves people in northeast Tennessee, southwest Virginia, northwest North Carolina and southeast Kentucky. Since Haas started in the newly created position six months ago, it’s been a whirlwind of activity. And yet, as she often points out, becoming trauma-informed is a journey, not a destination. Turning around a culture, especially a health culture that’s more familiar with doing things the “traditional” way rather than embracing change, will take time and lots of repetition.
Haas came to Ballad after several years with the Johnson City (TN) Police Department where she administered the Targeted Community Crime Prevention program and educated Johnson City and surrounding communities about the science of adverse childhood experiences and trauma-informed care. She and Dr. Andi Clements, a psychology professor at East Tennessee State University, developed the Johnson City System of Care for communities to use to integrate trauma-informed practices based on ACEs science. For a more detailed account of how she ended up at Ballad, read Becky Campbell’s article, Niswonger program aims to help traumatized children, in the Johnson City Press.
Following is a short Q-and-A with Haas about her first six months at Ballad, and her plans.
Q. What’s your overall goal?
A. My main goal is to develop a program for Ballad Health that advocates for trauma-informed practices in the community and in the Ballad Health system, and then educate and collaborate with partners inside and outside the hospitals to do so.
Q. What are the first steps you’ve taken?
A. I’ve started with Niswonger Children’s Hospital where, in the last four months, 218 clinical staff received an in-person two-hour training. At this point, all training is in person, not online. It’s important to talk about trauma-informed care face-to-face, because hospital staff deal with a high prevalence of trauma every day, and it creates secondary trauma in health care professionals that needs to be talked about.
Q. What feedback have you had?
A. I’m getting some good feedback from people who said their eyes are being opened, not only to the effects of trauma in patients, but also to how it affects them personally. Managers are reporting greater empathy in staff towards patients as we deal with a population with high rates of drug addiction.
Q. What exactly do you teach them in those two hours?
A. They learn what trauma is and how to integrate trauma-informed practices into their consciousness and work. We use the definitions and guidelines developed by the U.S. Substance Abuse and Mental Health Services Administration (SAMHSA), which is used by thousands of organizations around the country. I show them the Building Strong Brains video and the ACEs Primer video (ACEs = adverse childhood experiences). I provide some data about trauma, and then dive into the six pillars of trauma-informed care and provide examples so that the training leaves attendees with an expectation they are to use this information in daily settings.
Q. How long will it take to train everyone?
A. We’re planning on repeating what we did at Niswonger in four hospitals a year, so that’s a five-year plan. Funding for additional staff could shorten that.
 Q. What other ways are you working with people?
Q. What other ways are you working with people?
A. I’ve done some grand rounds in the hospitals and testified before the state legislatures. Here at Niswonger, we have First Friday lunches with nurse managers that have become a source of self-care for staff. Several managers report that staff now connect the dots between patient behavior and trauma. One manager and her Child Life team submitted an abstract to present at a healthcare conference on trauma -informed child life. Collectively we are rolling out as a healthcare system the D-E-F Protocol for Pediatric Care developed by Children’s Hospital of Philadelphia. This comprises reducing patient DISTRESS, providing EMOTIONAL SUPPORT and remembering the FAMILY. This trauma-responsive approach is helping health care workers tune into patients as a whole individual while they’re being treated for injury or disease.
Also, we’ve contacted numerous school systems and law enforcement agencies in the counties, to support their efforts to launch Handle With Care, where the police department notifies schools of all addresses where police have responded in the previous 24 hours to handle an incident, such as domestic violence. The schools don’t know what happened at the home, they just know that it’s likely to have been traumatic for the children at those addresses, so they check in with kids to see how they’re doing, offer help, and tell their teachers so that they understand if a kid is acting out or falls asleep in class.
Based on the incredible success we had in Johnson City, I’m working with schools to teach teachers and staff about trauma and trauma-informed practices and developing a menu of classroom interventions. This is part of a statewide movement that the Tennessee Department of Education is also integrating into schools. We want to use schools as a geographical hub for community health fairs, social services, etc., so that we bring all the services that children and families need to the schools.
We are also planning to work with local Chambers of Commerce to provide training for a trauma-responsive workforce and help them to understand about trauma in the workforce.
Of course, I enjoy working with law enforcement, and am excited about a recent request to provide trauma-informed policing training for the Bristol and Johnson City police departments as well as East Tennessee State University public safety officers.
Q. Are there any events coming up?
A. We’re having our first annual conference July 11. We’ll be covering topics such as trauma-informed health care and trauma-informed criminal justice. Some of the people who’ll be presenting include best-selling author Liz Murray, who’ll be telling her Homeless to Harvard story; and Dr. Stephanie Covington, who will be educating professionals how to integrate trauma-informed practices with “Recognize, Respond and Recover”. Dr. Andi Clements and I will be giving practical steps on how to develop a community of care. After lunch there are multi-disciplinary break-out tracks in the afternoon on trauma-informed community health, education and criminal justice. We want to create this area to be a national destination for people to learn about trauma-informed practices, and not just in health care.
Q. You sound as if you’re really, really busy, and the demand for the knowledge you’re providing is high. How are you taking care of yourself? Do you have an assistant?
A. I take long bike rides on my favorite trails, practice my faith, enjoy my family and grandchildren, and have requested a budget to add a staff member or two in the near future.





Comments (1)