
If the risk factors of Childhood Trauma | ACEs and Mental Illness are not treated at the same time as the addiction (aka substance use disorder), it is just about impossible for a person to successfully treat their addiction and succeed in long-term recovery.
Every week I receive calls and emails from family members and friends trying to find treatment for their loved one’s addiction,* aka substance use disorder. These kinds of phone calls and emails are heartbreaking. Their panic, anger, fear, frustration, sadness, desperation and anguish are palpable as they ask me:
- How can I make them get help? I’m afraid s/he’s going to die!
- What makes one place better than another?
- What do I do when they won’t accept my insurance (or my insurance doesn’t cover their program)?
- Why didn’t the last rehab work?
- S/he tried AA and gave up but what else is there?
- S/he gets out of treatment in 3 days, and I can’t find a safe place for him/her to go – what do I do?
What’s especially sad for me is that I receive the same kinds of calls and emails over and over and over and over, again. It should NOT BE THIS HARD to find effective treatment.
And, yet, it is. It’s terribly hard. So wrote a recent post on BreakingTheCycles.com to share what I consider to be seven key things a family member or friend needs to know when looking for addiction* treatment for their loved one or friend.
# 3 read:
Understand the five key risk factors for developing addiction
Understand how powerful the five key risk factors are to a person developing addiction. In other words, it takes misusing a substance to chemically and structurally change the brain, but it’s these five key risk factors that make one brain more susceptible to developing addiction than another brain. This helps explain why one in a group of friends drinking or using the same amount will develop addiction and the others will not. Understanding these risk factors will help you better understand the kind of treatment your loved one needs. These risk factors include:
- genetics (one can’t help their genetics, but it explains a big piece of the puzzle of how one person develops addiction and another does not when both are using/misusing the same amount – in fact, genetics is 40-60% of the reason a person misusing alcohol or other drugs goes on to develop addiction);
- childhood trauma (verbal, physical, emotional abuse, neglect…for some this is also ACEs – adverse childhood experiences) which resulted in toxic stress, which can change a child’s brain wiring (brain architecture), and if not addressed during treatment and continuing care is often a trigger to relapse);
- social environment (given a person's brain is wiring and mapping from birth, a child's social environment has a significant impact on that wiring and mapping -- a child's brain developing in a calm, nurturing environment vs. a chaotic, neglectful environment, for example);
- mental disorder (also a brain disorder and one that needs to be addressed if it’s still present [co-occurring] so as not to be a relapse trigger to use/misuse because of the mapping of the substance as a soother of the symptoms of the mental disorder – 40% of persons with addiction have a co-occurring mental disorder); and
- early use (the brain developmental processes occurring from ages 12 – 25 are deeply influencial in the development of addiction in the person misusing alcohol or other drugs during this time).
I then concluded #3 with the following:
I encourage you to pay particular attention to mental illness and childhood trauma | ACEs...
I encourage you to pay particular attention to the childhood trauma | ACEs and mental illness risk factors I mentioned above. Why? Because of the way the brain works, wires and maps as I described in #2, and how mental illness and the toxic stress caused by childhood trauma and ACEs changes that wiring and mapping.
Specific to childhood trauma | ACEs:
Time and again when I speak before audiences or talk one-on-one with individuals or engage in conversations with therapists and other medical professionals, the answer is, “No,” when I ask, “Have you heard of the ACE Study?” This continues to shock and sadden me because the ACE Study was conducted in the late 1990s, and yet, understanding and using this Study’s findings can have a profound impact on a person’s treatment and recovery success. To learn more about the ACE Study and ACEs and find an extensive list of resources, please check out Jane Steven's, founder/editor of ACEs Connection Network, post, "ACEs Science 101 (FAQs)." And check out her interview with Dr. Dan Sumrok in her article, "Addiction doc says: It's not the Drugs. It's the ACEs -- adverse childhood experiences."
And, I must say it again. If a person's childhood trauma | ACEs are not treated -- "healed" -- the profoundly negative impact on a person's addiction treatment and recovery can be huge because of the brain wiring and mapping that occurred around the trauma-related toxic stress triggering emotions and the reactionary coping skills that were mapped to stay safe in the midst of the childhood trauma | ACEs. Without treatment specifically geared to helping the person recover from their childhood trauma | ACEs, anything that triggers the deeply embedded trauma-related toxic-stress brain maps will continue to trigger the use of the substance that has mapped as the answer to, the soother for, those trauma-related toxic stress triggering emotions and reactionary coping skills.

Childhood Trauma | ACEs and the Addiction Connection is more easily understood when we understand how the brain develops and what influences that development.
Specific to mental illness:
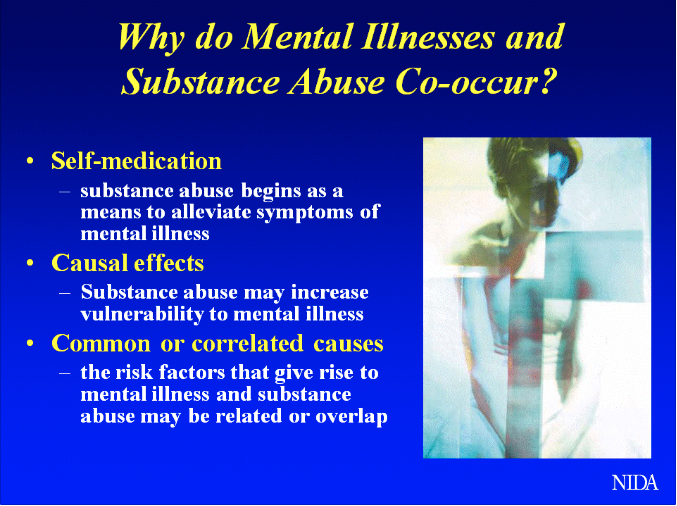
Having a mental illness and an addiction is to have two brain diseases (aka disorders); two diseases that both need to be treated at the same time. Think of it this way. If a person has diabetes and lung cancer, medical practice would require co-occurring treatment of these co-occurring medical conditions. And as I explained the importance of treating a person's childhood trauma | ACEs above as a key to their success in addiction treatment and recovery, so, too, is it important to treat their mental illness at the same time as their co-occurring addiction. To more fully understand this, I refer you to my post, "Co-Occurring Disorders Require Co-Occurring Disorders Treatment, and NIDA's image below.
To read the full post, click 7 Things to Know When Looking For Addiction Treatment.
_________________________
*NIDA (the National Institute on Drug Abuse) continues to use the term addiction and defines it as a chronic, relapsing brain disease. However, as NIDA also writes, “addiction” is not considered a specific diagnosis in the fifth edition of The Diagnostic and Statistical Manual of Mental Disorders (DSM-5), which was updated in 2013. DSM-5 replaces the categories of substance abuse and substance dependence with a single category: substance use disorder. Given the general public still thinks of a person’s dependence on alcohol or other drugs as addiction, I used this term in this article.






Comments (4)