How one rural clinic addressed its patients’ complex health and social needs successfully—and cut emergency room use and costs drastically.
Nestled near the Blue Ridge Mountains, the Clinics serves Henderson and Polk counties, agricultural communities with many residents who live in rural areas or are migrants living in tent camps. Thirty-eight percent of the adult population live in families with incomes below 200% of the federal poverty line.
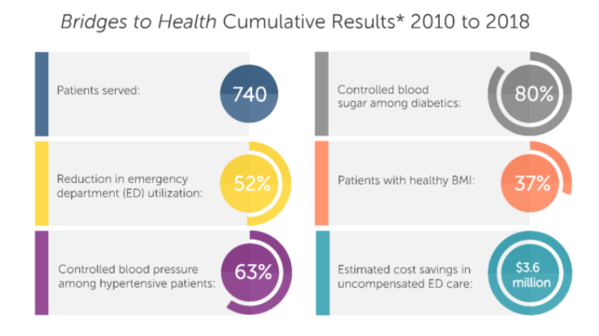
While volunteering with the Clinics, Steven Crane, M.D., discovered that about 255 low-income, uninsured patients in the prior year accounted for 90% of the emergency room billing at a county hospital with a population of 100,000 people.
“These were very complex patients. Almost all of them had severe mental health or behavioral problems, or both,” Crane says. Seventy percent of the patients had experienced adverse childhood experiences such as poverty or abuse that can affect mental health and learning for a lifetime. They were typically uninsured, and had difficulty making and keeping appointments and following medical advice, compounding severe medical issues and turning into “frequent flyers” to the ER, as Crane puts it.
The Clinics are a literal haven, too, especially for those living in turbulent households or without a place to live. “For many of these folks, it was the only safe place they had. Some would come to sleep here during the day because they couldn’t at home,” Crane says.
To read more of Catherine Malone'a article, please click here.

Comments (0)