Kidsdata and the California Department of Public Health (CDPH) have partnered to share important new measures of maternal mental health before and after a live birth from the Maternal and Infant Health Assessment (MIHA) survey. A woman's emotional well-being during this time is central to her health and to her infant's development. Depression during and after pregnancy is a serious medical condition that requires culturally appropriate and trauma-informed support and treatment.
Guest authors, Christine Rinki and Amina Foda, Research Scientists with the California Department of Public Health, share important findings about symptoms of depression among women who recently gave birth in California:
Symptoms of depression during and after pregnancy
According to a recent Data Brief (PDF) from the California Department of Public Health's Maternal and Infant Health Assessment (MIHA) survey, about one in five women who give birth in California experience symptoms of depression during or after their pregnancy.
Although relatively minor changes in mood the first few days after childbirth are common, depression that arises during or after pregnancy is a mood disorder characterized by intense feelings of sadness, anxiety or despair that last for two weeks or longer and prevent women from doing their daily tasks.
If untreated, depression during or after pregnancy increases the risk of cognitive and emotional development problems in infants, and may result in fundamental changes in the brain that can have lasting effects into childhood. Depression occurring after the baby is born can negatively impact women's breastfeeding practices and ability to bond with their infants. Importantly, depression at any point during or after pregnancy increases the risk that women could develop chronic depression or die by suicide, which in turn have profound impacts on children.
Thankfully, with the appropriate care, most women can experience a full recovery. Best practices to address maternal mental health include screening for depression throughout prenatal and postpartum care, and increasing the availability of services that are affordable, culturally and linguistically appropriate, and that acknowledge the history of trauma common among women with depression.
Prenatal and postpartum symptoms of depression in California
In California, 14.1% of women experienced prenatal symptoms of depression and 13.5% experienced postpartum symptoms of depression. Many, but not all, women who experienced symptoms of depression would be diagnosed with clinical depression.
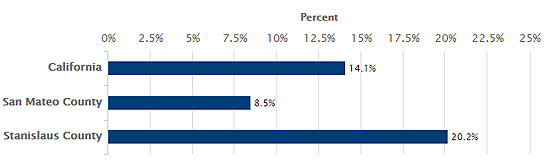
There was substantial geographic variation among counties with data. Prenatal symptoms of depression ranged from 8.5% in San Mateo County to 20.2% in Stanislaus County, while postpartum symptoms of depression were 9.8% in Yolo County and 18.8% in San Joaquin County.
Prenatal Symptoms of Depression
See data on prenatal symptoms of depression »
See data on postpartum symptoms of depression »
Prenatal symptoms of depression: Important, but often overlooked
Despite the serious risks associated with prenatal depression, including low birth weight, premature delivery and changes in infant brain development, its importance is often overlooked. MIHA results (PDF) indicate that prenatal symptoms of depression often precede postpartum symptoms of depression in women. In California, 53% of the women who experienced prenatal symptoms of depression went on to report them in the postpartum period. In contrast, only 7% of women without symptoms of depression during pregnancy experienced them after pregnancy. In order to have the best chance of improving outcomes for the mother and infant, routine screening and treatment for depression should begin early in pregnancy, a time when women have increased contact with the health care system.
Disparities in prenatal symptoms of depression
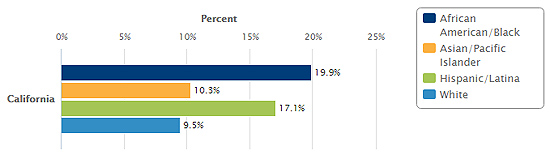
Though symptoms of depression during and after pregnancy can affect women regardless of their background or circumstances, some groups in California experience them at disproportionately high levels. Women who are Black or Latina had higher rates of symptoms of depression compared to other racial or ethnic groups. During pregnancy, symptoms of depression were twice as common for Black (19.9%) and Latina (17.1%) women compared to White (9.5%) and Asian/Pacific Islander (10.3%) women. Reports of prenatal and postpartum symptoms of depression were highest among women with incomes below poverty (20.7% and 18.2%, respectively), and declined as income increased.
Prenatal Symptoms of Depression by Race/Ethnicity
See data on disparities in prenatal and postpartum symptoms of depression »
Programs that address perinatal emotional and mental health
The Maternal, Child and Adolescent Health Division of the California Department of Public Health strives to improve maternal emotional and mental health by tailoring primary prevention to address the social factors that lead to poor emotional and mental health and to promote individual protective factors. Additionally, many MCAH Division programs screen for symptoms of depression using validated tools, and provide appropriate referrals and support for women in need of care. For example, the Black Infant Health Program conducts group sessions with complementary case management that provide social support while helping women develop skills to reduce stress, enhance emotional well-being and develop life skills in a culturally affirming environment that honors the unique history of Black women. The California Home Visiting Program funds home visiting models throughout the state that use a strengths-based approach to enhance the mother-baby relationship. Home visitors address family needs such as financial struggles, relationships, and navigating the health care system, while support groups and mental health consultation directly address emotional well-being.
Striving for equity in perinatal emotional and mental health
The underlying causes of the maternal mental health disparities identified in the MIHA Data Brief are multifaceted. For example, Black and Latina women in California experience higher levels of risk factors for depression such as poverty and childhood hardships compared to other racial and ethnic groups. Institutional racism (the practices of social and political institutions that result in unfair treatment of Black, Latina and other minority groups) likely plays a role in explaining the concentration of risk factors, and the subsequent racial and ethnic disparities in symptoms of depression. Achievement of emotional and mental well-being for all California women during and after their pregnancies can have profound societal impacts. Action to address social factors can improve outcomes for low-income and minority families.
Comments (0)