 Simultaneously making changes at the organizational level and building alliances across sectors for larger system change, Father Jeff Putthoff, SJ, and Dr. Jeffrey Brenner realized they had to dig deeper — beyond symptoms to root causes — to understand the struggles they were witnessing in Camden, NJ. What they found were ACEs.
Simultaneously making changes at the organizational level and building alliances across sectors for larger system change, Father Jeff Putthoff, SJ, and Dr. Jeffrey Brenner realized they had to dig deeper — beyond symptoms to root causes — to understand the struggles they were witnessing in Camden, NJ. What they found were ACEs.
Putthoff, a Jesuit priest known locally as “Father Jeff,” is a fireplug of purpose under his casual uniform of cargo shorts and sweatshirt, earbuds slung around his neck, a blue bicycle his preferred mode of transport. He is voluble and passionate on the subject of his city. Since 2000, Father Jeff has directed Hopeworks N’ Camden, an organization that offers in-school and out-of-school youth GED classes and web-site design instruction—skills intended to parlay directly into jobs or college.
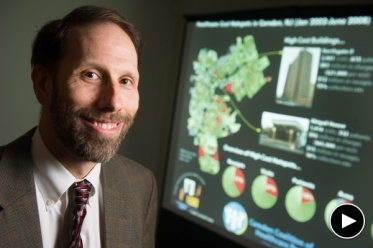
Brenner is equally driven—a physician/scholar/prophet in a slightly rumpled suit, with a calendar so crammed he must set a smartphone alarm to keep his days on track. He is founder and executive director of the Camden Coalition of Healthcare Providers and the recipient of a 2013 MacArthur “genius” grant. In 2011, he was profiled in The New Yorker, which chronicled his innovative plan to shrink the cost of health care by focusing on the highest-risk patients, providing them with team-based interventions to keep them out of hospitals, and by helping them manage chronic illnesses and social/emotional needs.
But it wasn’t until the last three years that each man learned of the CDC Adverse Childhood Experiences Study, whose first study was published in 1998, and began to apply its lessons to his work. That study, of more than 17,000 Kaiser Permanente members in California, showed that early childhood adversity—including neglect, physical and sexual abuse and parental abandonment—was both widespread and corrosive to long-term physical and mental health. Trauma, the study implied, leaves tracks in the brain and lingers in the body. Stress can literally make people sick.
Putthoff saw the symptoms of that trauma every day. Camden earned the dubious title of “most violent city in America” in 2012, when there were 67 homicides among its 77,000 residents. That year, someone in Camden was shot, on average, every 33 hours. Two out of five Camden residents live below the poverty line. The streets are pocked with nearly 4,000 abandoned homes.
“I’ve been here [in Camden] 16 years,” Putthoff said. “I’ve been chasing the symptoms all those years, trying to change people’s behavior, get them jobs, get people in school. The dawning realization was that we were not dealing with the cause.”
Hopeworks N’ Camden provides training programs in a trauma-informed environment
Putthoff could see how frustration and hopelessness were wearing on the Hopeworks staff—10 full-time and four part-time employees who work to boost students’ reading skills and teach them web site design and GIS (geographic information systems, or digital mapping). They also reinforce workplace norms such as appropriate dress and consistent, on-time attendance.
![Father Jeff Putthoff [Photo: Yong Kim, Philly.com] Father Jeff Putthoff [Photo: Yong Kim, Philly.com]](http://acestoohigh.files.wordpress.com/2014/09/aputthoff.jpg?w=373&h=254)
“About three years ago, I noticed that my staff were being really mean to each other, saying things like, ‘Ann, you’ve been late twice in a month; what’s the matter with you?’ It was getting nasty,” Putthoff said.
“It was classic secondary trauma. The organization needed to heal.”
After reading more about adversity and stress, Putthoff diagnosed the toxic workplace atmosphere: “It was classic secondary trauma. The organization needed to heal.”
Putthoff learned about The Sanctuary Model, developed in the Philadelphia area in the early 1980s. The model is a blueprint for organizational change to create a trauma-informed community that includes not only the people seeking treatment or services, but those who provide those services. Organizations that wish to follow the Sanctuary Model make a commitment to undergo intensive training, staff development and rigorous reflection to change behavior, attitudes and practices. Three years ago, Hopeworks began that process.
Today, the principles of trauma-informed care infuse everything that happens at Hopeworks. Each morning, in a room on the second floor of Hopeworks’ headquarters, an unassuming row house in the Pyne Point neighborhood, both staff and youth gather for “the huddle,” a check-in designed to clarify feelings and set intentions for the day.
First, everyone takes three deep breaths “to root ourselves in our bodies,” Putthoff explained. Then each participant, in turn, asks the person on his or her left four questions: “How are you feeling? How do you want to feel at the end of the day? What’s your goal for today? Who can help you with that?”
“It’s powerful to acknowledge feelings,” Putthoff said. But it’s equally important to name a specific goal and seek out someone else as a resource—for instance, ‘I’m going to finish exercise two in my GED book, and I’ll get Jay to check my work.'”
“What we’re saying is, ‘You can have your feelings and function,’” Putthoff said.
Dan Rhoton, Hopeworks’ chief impact director, explains trauma-informed care this way: Imagine two youth, Hakim and Maria. Hakim routinely shows up late; he flouts the rules by checking his cell phone incessantly during training sessions. He demands, “How long until I get my stipend?” Maria, on the other hand, reports on time every day and stays focused; instructors learn that she’s caring for her siblings because her mother was deported. A conventional approach would term Hakim “a failure” and Maria “a hero,” Rhoton said.
“But Hakim and Maria are the same. He’s checking his phone because his five-year-old brother is alone at home. He needs his stipend because that’s how he pays for groceries. Who you see depends on the questions you ask.”

This article about Camden, NJ is one of several profiles of communities that are becoming trauma-informed. They are published together in the Community Resilience Cookbook.
_________________________________
Hopeworks staff have learned to pose different questions. All youth take the ACE inventory, as well as an education survey that asks questions such as, “Have you felt safe at school?” in an effort to uncloak the reasons for low grades or dropping out. In contrast to programs with strict three-tardies-and-you’re-out policies, Hopeworks is more flexible. “We ask, ‘How can we help you to be successful?’” said Danyelle Austin, the program’s academic success director.
And the big question, the one that applies not just to Hopeworks youth but to all residents and workers in this struggling city, is not “What’s wrong with you?” but “What happened to you?”
“What happened to us,” says Putthoff, “is that we’ve chosen to live and work in the poorest, most violent city in the country. But healing is available.”
Putthoff is trying to spread that word beyond the walls of Hopeworks. In May 2013, Putthoff and others hosted a Trauma Summit featuring keynote speaker Sandra Bloom, co-director of the Center for Nonviolence and Social Justice at Drexel University’s School of Public Health; she is co-creator of the Sanctuary Institute.
The chief of police attended the Trauma Summit. So did numerous neighborhood activists, clergy members, teachers and citizens eager to learn more about what ails Camden and how to fix it. Putthoff followed the summit with a series of “Trauma Triangle” workshops to further participants’ learning about the effects of adversity and ways to boost resilience. Now he is working to gather a cluster of Camden organizations to be part of a “Healing 10”—agencies that will commit to the Sanctuary Model, practice trauma-informed care and work together—in collaboration, not competition—across disciplines, to repair this broken city and its people.
A year later, that work is starting to gain traction; Drs. Robert Anda and Vincent Felitti, co-investigators of the ACE Study, spoke at Camden community events in the spring of 2014. A small group of leaders committed to the idea of the Healing 10 has been meeting regularly with Putthoff, and more than 70 people filled the room for a three-hour training on the Sanctuary process. Putthoff hopes that momentum will continue at the next Trauma Summit to be held next week.
Meantime, Hopeworks continues applying the lessons of ACEs to its own daily practice, and sharing that knowledge with others. A recently formed youth trauma team, trained in ACEs theory, has presented to schools, community centers and other sites. The most powerful moments, Putthoff says, come when the youth tell their stories. One boy talks frankly about being stabbed by his father; a girl discloses her history of self-injury and drug use. They describe how understanding ACEs has helped them heal and given them a new framework for seeing the world.
“We’re humanizing ACEs,” Putthoff said. “People think: Oh, that’s the group of youth that’s a problem. They’re the ‘other.’ The youth really cross that boundary because they share their stories. That’s the gist of Felitti’s [message]: in talking about what happened to you, a great power begins to move.”
Education leaders in the city are also starting to embrace ACE-informed practices. The Catholic Partnership Schools, a coalition of five Camden schools, hosted an Education Summit in 2013 that brought 300 educators to hear Paul Tough, author of How Children Succeed: Grit, Curiosity, and the Hidden Power of Character, talk about the impact of poverty on children’s ability to learn. In some of those schools, teachers are using mindfulness meditation, “peace corners”, and soothing music to help children manage their emotions and learn resilience.
A second Education Summit the following spring focused on “Self-Control, Poverty, Social and Emotional Development, and the Roles They Play in Raising our Children.” It featured University of Pennsylvania professor Angela Duckworth, who has written widely about the role of grit in determining children’s success.
While Putthoff has allies in town—the chief of police, other human service providers and the CEO of the Camden District Council Collaborative Board, which convenes groups of residents, educators and law enforcement officials to address crime and community issues–there is not yet a citywide network that shares the language of ACEs, the understanding of trauma and a commitment to build Camden’s resilience through long-term collaboration.
“I feel exhausted. I wish I could go around and give everyone a shot of penicillin,” Putthoff says. “But there’s not a vaccine. The change is cultural. I want to offer people an understanding of the symptoms of trauma, an understanding of where that’s coming from. People understand being hurt. I see this as an incredible way to connect with people and bring resources together.”
The ACE-informed physician changes his practice
Across town, on the other side of the freeway, Brenner and his staff are also practicing what they’ve learned from emerging biomedical research on adversity and long-term health.
Several years ago, Brenner’s staff interviewed a group of “high-utilizing clients”—that is, middle-aged adults whose chronic illnesses resulted in frequent emergency department visits and hospital stays. It turned out that this group had a high level of early-life trauma. That data eventually led Brenner to the CDC’s ACE Study.
“It opened up a whole new lens on all our work,” he said. “The ACE Study fills a gap” between the biology and physiology of stress and the ways that stress gets played out in adult decision-making.
“Alcohol, substance abuse, violence: poverty is full of bad choices,” Brenner said. “But those are coping strategies for chronic stress overlaid on early life trauma.”
“So much awful stuff happens from birth to death here [in Camden], ranging from physical violence to tremendous chaos in people’s families, not knowing where your next meal is coming from, substandard housing, unsafe schools…It’s all-encompassing.”
In an interview, Brenner recalled a patient he saw in his first year of practice, when he was just 28. The woman had diabetes; she suffered a foot ulcer and frequently came to his office with skyrocketing blood-sugar counts. “I would give her state-of-the-art medication, but I couldn’t get her better,” Brenner said. “Finally she came in one time and I put the chart down and said, ‘Who are you?’”
The patient, it turned out, was a retired kindergarten teacher, raised in the South; she was widowed, depressed and still suffering the effects of early-childhood trauma. “You realize, in medical care, how little we really know people, how ill-equipped we are to pull their stories apart. I was practicing with half a stethoscope and one hand tied behind my back,” he said.
Today, Brenner practices differently, both as a physician and as a manager. He puts the lessons of ACEs to work in his own organization, the Camden Coalition of Healthcare Providers. “The people attracted to helping professions tend to have high ACE scores,” he explains. “The ACE study made sense of why certain people were not responding well to doing this work, why they were getting enmeshed with clients and patients and with each other.
“We’re much more focused now on…working with the staff that we have” to help them understand and change destructive patterns of behavior, Brenner said.
In one of the coalition’s practices, the staff is working on a plan to screen all patients for ACEs, a prospect Brenner said unnerves some physicians because it challenges the medical model they’ve been taught. What’s needed, he said, is a simple ACE-screening framework, like those used to assess for depression or substance abuse, that could be used by frontline staff. Meantime, the coalition created a short animated video showing the relationship between early childhood trauma and emergency room use.
The priest and the physician continue to join forces; when CCHP brought on 10 new AmeriCorps volunteers in August 2014, Putthoff and his youth trauma team took part in their orientation, training the volunteers along with new CCHP staff in ACE fundamentals, trauma and resilience.
Brenner predicts it will take another generation for physicians to learn about and embrace the ACE Study and change their practices in response. “The trauma-informed model has not yet made it over to medicine. For the medical community, it is the biggest of paradigm shifts. But it’s how we are going to have to breathe.”
Brenner, like Putthoff, believes that the next step is to take the trauma-informed approach to a broader group of practitioners in Camden—not only in medicine, but in law enforcement, juvenile justice, education and human services. “We’re all scratching our heads about how to widen the circle,” Brenner said. “In the meantime, I just want to make sure that we know what trauma-informed means here, that we’re doing everything we can.”
___________________
This is one of several articles about how different towns, cities, states and provinces are beginning to embrace an ACEs movement and become engaged in preventing/treating ACEs and promoting resilience. They were done as part of a Community Resilience Cookbook, produced by the Health Federation of Philadelphia with support from the Robert Wood Johnson Foundation.



Comments (0)