Dr. Raul Gutierrez, a pediatrician in the San Francisco Bay Area, said he and his fellow clinicians see constant fear and its health consequences every single day among the largely immigrant and Latino population they serve. It’s all the result of anti-immigrant policies and the news cycle that feeds the fear.

“It is almost inescapable with the repercussions of immigration policy on the radio, television, social media and from friends and family,” Gutierrez told the 69 participants in a recent ACEs Connection webinar “The Trauma Toll on Pediatric Immigrants, Refugees and their Families” that took place on Dec. 14, 2018.
And for Gutierrez, who grew up in the border city of Brownsville, Texas, it’s also personal. “There was a recent story about American citizens along the border being denied passports. Their citizenship was being called into question because their birth was via the assistance of a midwife, and some [of the midwives] were accused of falsifying birth certificates,” said Gutierrez. “So, fear is what I felt as I wondered if any of my relatives were born with the help of a midwife, and whether their passports or citizenship would be called into question.”
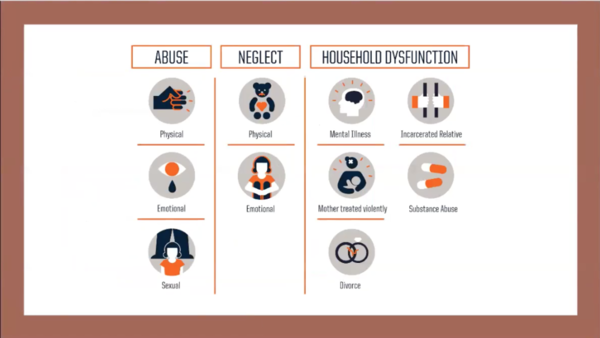 And how can clinicians understand what their young immigrant patients are experiencing? Gutierrez, a clinician who is the cofounder and director of the BRIDGES Clinic at Zuckerberg General Hospital in San Francisco, and also works in Oakland at La Clnica de la Raza’s school-based health centers, had some suggestions for the people who participated in the webinar. He pointed out that the original questions used as part of the landmark Centers for Disease Control and Prevention/Kaiser Permanente Adverse Childhood Experiences Study might not capture the experiences of immigrant children and their families. Pointing to a slide that illustrates the features of the original 10-question ACE survey, Gutierrez asked, “Can we extend the notion of incarceration to include the experience of being detained by the Immigration and Customs Enforcement (ICE)?”
And how can clinicians understand what their young immigrant patients are experiencing? Gutierrez, a clinician who is the cofounder and director of the BRIDGES Clinic at Zuckerberg General Hospital in San Francisco, and also works in Oakland at La Clnica de la Raza’s school-based health centers, had some suggestions for the people who participated in the webinar. He pointed out that the original questions used as part of the landmark Centers for Disease Control and Prevention/Kaiser Permanente Adverse Childhood Experiences Study might not capture the experiences of immigrant children and their families. Pointing to a slide that illustrates the features of the original 10-question ACE survey, Gutierrez asked, “Can we extend the notion of incarceration to include the experience of being detained by the Immigration and Customs Enforcement (ICE)?”
“Can deportation or forced displacement be considered some form of household dysfunction?” he continued. “And how do racism and xenophobia, whether experienced personally or in the community, fit into this model?” he asked. Some pediatricians are already including more questions on ACE surveys they give their patients. Those questions address racism and losing a family member to deportation, as well as other questions that capture the adversities commonly experienced by the populations they are serving.
Gutierrez also discussed how federal policies that target immigrants can make them feel less inclined to go to public places, use parks or seek health care.

To allay fears that can play out in keeping immigrant families from seeking health care, Dr. Heyman Oo, a pediatrician with Marin Community Clinics, described the kinds of visuals, handouts and signs a clinic can use to create an atmosphere of safety for newcomers and immigrant families. They include handouts in Spanish about organizations that provide everything from housing to legal assistance, and a notice about a weekly community health fair and farmers market, where families can get a bag of free food.
Oo also showed participants examples of “red cards” that advise patients of their rights. These can be slipped under the door should immigration authorities show up at their house. “They’re basically portable, little cards that you can have in the waiting room, have in the clinical room. People can use them as a way to communicate if someone shows up at their door. They don’t actually have to open their door,” explained Oo.
 Recognizing that the red card might be triggering, Oo told participants: “I always give it out and say, ‘It may not be appropriate for you, but if you know anyone in your apartment complex, it may be useful.’” She also suggests posting signs in multiple languages that include the same information around the clinic and exam rooms.
Recognizing that the red card might be triggering, Oo told participants: “I always give it out and say, ‘It may not be appropriate for you, but if you know anyone in your apartment complex, it may be useful.’” She also suggests posting signs in multiple languages that include the same information around the clinic and exam rooms.

Dr. Nick Nelson is the co-director of the Human Rights Clinic at Highland Hospital in Oakland, Calif. His patients are adults who have experienced multiple ACEs and recent trauma. Part of his work is documenting the physical and psychological imprints of trauma and torture. He reviewed various physical signs of torture and then described how, because of stigma, psychological trauma is expressed indirectly in many cultures, often through physical symptoms. He told the story of one patient who had lost about 100 pounds over six months.
“Everyone assumed he had some form of metastatic cancer,” recalled Nelson. However, after numerous diagnostic tests turned up no answers, one doctor asked the patient if he had ever been tortured. “And that was when they learned that he had actually been imprisoned in Yemen for three months, had been tortured extensively by the government, and all of his symptoms related to the psychological sequelae of those experiences.”
To learn more about the speakers’ presentations, click here to view the recording of the webinar, and see the attached slide presentations.






Comments (0)